Coffee, Acid Reflux, and GERD: What Research Says
Introduction to Coffee and Acid Reflux

Few rituals are as universal as the morning cup of coffee. For many, it’s a moment of focus and energy. But for others, that same ritual sparks an uncomfortable burn rising in the chest — a sensation often linked to coffee and heartburn. Is coffee really the villain behind acid reflux, or is the connection more complicated than it seems?
At a Glance: Coffee & Acid Reflux
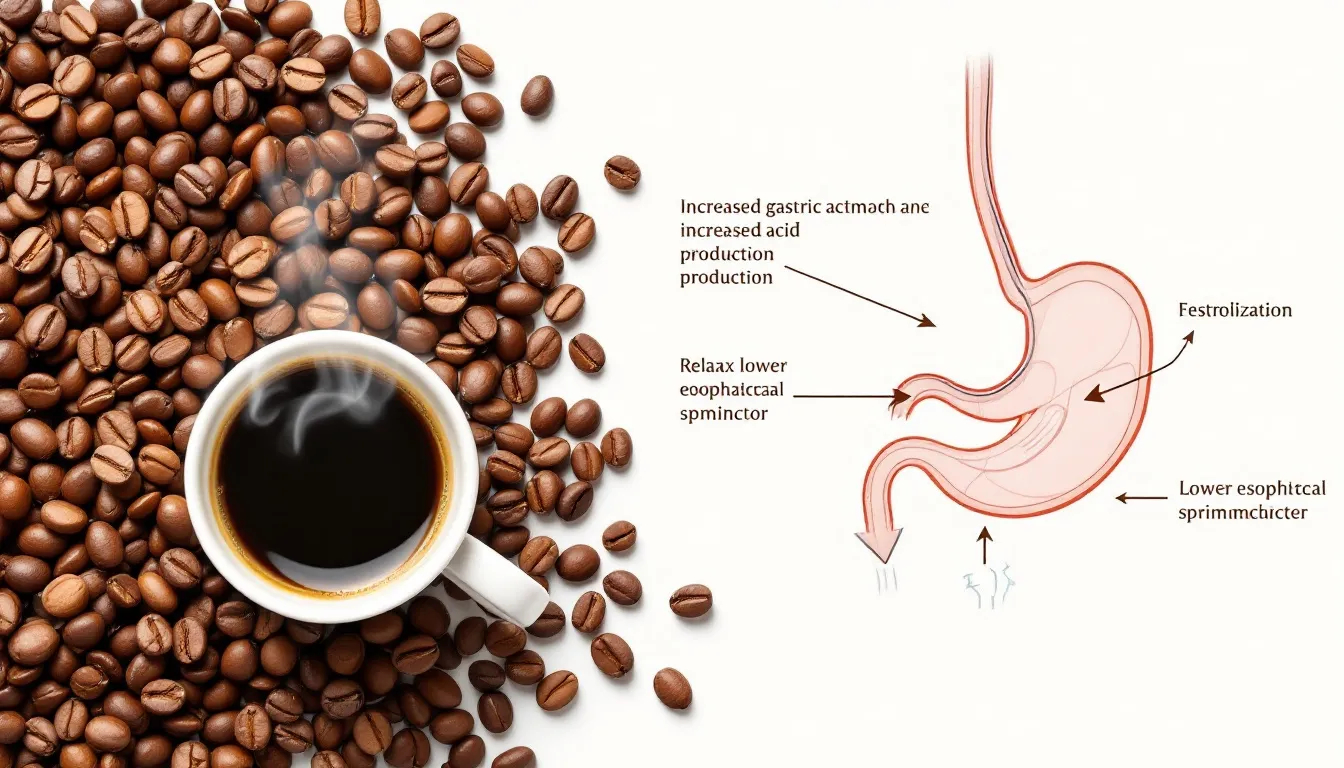
- Coffee may trigger acid reflux in sensitive individuals by stimulating stomach acid and relaxing the lower esophageal sphincter (LES).
- Sensitivity to coffee and GERD varies—some people tolerate several cups daily, while others feel discomfort after just one sip.
- Choosing dark roast coffee, adding milk, or avoiding coffee on an empty stomach may help reduce reflux symptoms.
- Recent studies show mixed results: some find no strong association between coffee and GERD, highlighting the need for a personalized approach.
- If heartburn or reflux occurs more than 2–3 times per week, consult a gastroenterologist for evaluation and treatment.
For millions of people worldwide, the day begins with the comforting aroma of coffee. Yet, for some, that same cup comes with an unwelcome side effect: acid reflux—the burning sensation that occurs when stomach acid flows back into the esophagus.
The link between coffee and digestive health has been debated for decades. While many assume coffee automatically causes reflux, the truth is far more complex. Some coffee drinkers experience instant heartburn after a single cup, while others can enjoy several mugs without issue. Recent research suggests that coffee’s role in gastroesophageal reflux disease (GERD) is not as straightforward as once believed.
In this guide, we’ll break down the science behind coffee and acid reflux, explore the latest medical findings, and share practical solutions for coffee lovers who want to enjoy their daily brew without discomfort. Whether you deal with occasional heartburn or live with chronic GERD, understanding how coffee affects reflux can help you make smarter, healthier choices—without giving up your favorite beverage entirely.
Before we decide whether coffee is a friend or foe, it helps to understand what acid reflux and GERD actually are—and why the lower esophageal sphincter (LES) plays such a central role. Once the mechanics are clear, the coffee connection makes much more sense.
Understanding Acid Reflux and GERD

Acid reflux, often felt as heartburn, happens when stomach acid backs up into the esophagus, causing a burning sensation in the chest. When this occurs frequently or becomes chronic, it is known as gastroesophageal reflux disease (GERD)—also called gastro-oesophageal reflux disease in some regions. GERD is widespread, affecting about 25% of adults worldwide, making it one of the most common digestive disorders globally.
The Lower Esophageal Sphincter (LES): The Valve That Matters
The lower esophageal sphincter (LES) is a circular muscle at the junction of the esophagus and stomach. When working properly, the LES stays closed except when swallowing, preventing acid from escaping upward. However, if the LES weakens or relaxes inappropriately, acidic stomach contents can rise into the esophagus and irritate its delicate lining. Caffeine, alcohol, obesity, pregnancy, and large meals are some factors known to trigger this relaxation.
Symptoms of Acid Reflux and GERD
GERD symptoms can vary, but the most common include:
- Heartburn — a burning feeling in the chest, often after meals
- Regurgitation — sour or bitter acid rising into the throat or mouth
- Chest pain — sometimes mistaken for cardiac problems
- Difficulty swallowing (dysphagia)
- Chronic cough, hoarseness, or a sensation of a lump in the throat
Symptoms tend to worsen when lying down or bending over, since gravity no longer keeps stomach contents in place.
The Growing Prevalence and Risks
The prevalence of GERD has risen significantly in recent decades, with most adults experiencing at least occasional heartburn at some point. But if symptoms occur more than twice a week, it may signal a more serious condition that needs medical attention. Untreated GERD can lead to complications such as esophagitis (inflammation), ulcers, strictures, or in rare cases, even require surgery.
Why This Matters for Coffee Drinkers
Understanding the mechanics of reflux explains why some foods and beverages—coffee included—can act as triggers. But it’s important to recognize that acidity alone doesn’t determine reflux risk. Factors like caffeine content, roasting style, brewing method, and individual sensitivity all play a role in how coffee interacts with digestive health.
Common GERD Symptoms vs Red-Flag Symptoms
| Common GERD symptoms | Red-flag symptoms (seek medical care) |
|---|---|
| Heartburn (burning chest sensation) | Chest pain with shortness of breath, sweating, or pain radiating to arm/jaw |
| Regurgitation with sour or bitter taste | Difficulty swallowing (dysphagia) or pain with swallowing (odynophagia) |
| Acidic taste in the mouth | Unintentional weight loss |
| Worse after large meals or when lying down | Persistent vomiting or inability to keep fluids down |
| Intermittent cough or hoarseness | Signs of bleeding: black/tarry stools, vomiting blood, or “coffee-grounds” vomit |
| “Lump in throat” sensation | Iron-deficiency anemia or severe fatigue related to blood loss |
Table 1. Common GERD symptoms are often manageable with lifestyle changes and over-the-counter remedies. Red-flag symptoms may indicate complications and warrant prompt evaluation by a healthcare professional.
With the basics of acid reflux and GERD in mind—including how the lower esophageal sphincter works and the symptoms that may require medical attention—it’s easier to see why certain foods and drinks can make a difference. One of the most debated is coffee. While often blamed for heartburn, coffee also comes with an impressive list of potential health benefits. Understanding this balance is key to deciding whether your daily brew is a risk, a reward, or sometimes both.
So, does coffee actually cause acid reflux—or can it still be part of a healthy lifestyle?
The Connection Between Coffee and Health Benefits

Coffee isn’t just a comfort drink; it’s a phytochemical-rich beverage containing caffeine, chlorogenic acids, diterpenes (cafestol and kahweol), trigonelline, and hundreds of other bioactive compounds. Together, these contribute to both health-promoting effects and, in some cases, digestive discomfort.
☕ Coffee’s Key Health Benefits
- Metabolic support: Linked to a 15–30% lower risk of type 2 diabetes in large cohort studies, thanks to chlorogenic acids that improve glucose metabolism.
- Cardiovascular health: Moderate intake may reduce the risk of stroke and coronary heart disease due to coffee’s antioxidant and anti-inflammatory compounds.
- Cognitive function: Caffeine acts as an adenosine receptor antagonist, improving alertness and potentially protecting against Alzheimer’s and Parkinson’s disease.
- Weight management: Caffeine can boost metabolism and fat oxidation, supporting modest weight control when paired with healthy diet and exercise.
Evidence for Health Benefits
Metabolic health: Multiple cohort studies, including large-scale analyses in the New England Journal of Medicine and BMJ, show that people who consume 3–5 cups of coffee daily have a 15–30% lower risk of type 2 diabetes compared to non-drinkers. The protective effect is thought to come from chlorogenic acids, which improve insulin sensitivity and glucose metabolism.
- Cardiovascular health: Meta-analyses have linked moderate coffee consumption to a reduced risk of stroke and coronary heart disease, possibly due to antioxidant and anti-inflammatory properties of polyphenols.
- Cognitive benefits: Caffeine acts as an adenosine receptor antagonist, reducing fatigue and improving alertness. Long-term studies also suggest a potential protective role against neurodegenerative diseases such as Alzheimer’s and Parkinson’s.
- Weight management: Caffeine can increase thermogenesis and fat oxidation, supporting modest weight control when paired with a healthy diet.
Why Benefits Aren’t Universal
Despite these findings, not everyone reaps coffee’s rewards. Genetic polymorphisms in CYP1A2—the enzyme that metabolizes caffeine—determine whether someone is a fast or slow metabolizer. Slow metabolizers often experience greater side effects (palpitations, anxiety, reflux) and may not gain the same cardiovascular protection seen in population studies.
For those with GERD or acid reflux, caffeine and natural acids can trigger symptoms by relaxing the lower esophageal sphincter (LES) or irritating the esophageal lining. Yet intriguingly, some research suggests coffee may actually stimulate gastric motility and improve digestion in certain individuals—showing how nuanced its effects can be.
Balancing Health Benefits with Reflux Risk
To maximize health benefits while minimizing reflux:
- Track your own sensitivity (food/symptom diary).
- Choose darker roasts, which are lower in chlorogenic acids and gentler on the stomach.
- Add milk, which buffers acidity and slows gastric emptying.
- Avoid consuming coffee on an empty-stomach to reduce direct acid exposure.
In short: Coffee may lower your risk of diabetes, stroke, and cognitive decline—but if you’re prone to reflux, the way you drink it matters as much as whether you drink it.
While these findings highlight why coffee is often celebrated as a health-promoting beverage, there’s another side to the story. For individuals sensitive to acid reflux or GERD, the very same compounds that make coffee beneficial—like caffeine and chlorogenic acids—may also contribute to discomfort. To understand this balance fully, we need to look at how coffee can sometimes trigger reflux symptoms.
How Coffee May Trigger Acid Reflux

The relationship between coffee and acid reflux isn’t explained by a single factor. Instead, several physiological mechanisms interact to increase the likelihood of symptoms for sensitive individuals. Coffee affects the digestive system in ways that involve acid production, muscle relaxation, timing of consumption, and brewing methods—all of which can tip the balance toward heartburn in some people.
1. Stimulation of Gastric Acid Production
When you drink coffee, especially caffeinated coffee, it directly stimulates the stomach’s acid-producing cells and indirectly raises acid output through hormones such as gastrin, a key regulator of digestion. This surge in gastric acid can irritate the stomach and increase the risk of reflux episodes.
Certain compounds in coffee beans, particularly in dark roasts, can further influence how much acid the stomach produces.
While this doesn’t affect everyone equally, those predisposed to reflux may experience noticeable discomfort.
2. Coffee’s Natural Acidity
Coffee’s pH typically ranges from 4.85 to 5.13, making it moderately acidic—though still less acidic than citrus juices. The acidity alone doesn’t tell the whole story, but chlorogenic acids and other compounds found in coffee beans can irritate sensitive digestive tissues and increase stomach acid production.
Interestingly, dark roast coffees develop more of a compound called N-methylpyridinium (NMP) during roasting. NMP may actually reduce gastric acid secretion, which explains why some people tolerate dark roast better than light roast. This highlights how roast level can significantly change how coffee interacts with reflux.
3. Relaxation of the Lower Esophageal Sphincter (LES)
Perhaps the most significant mechanism is caffeine’s ability to relax the LES—the muscular valve that normally prevents stomach acid from moving back into the esophagus.
Once relaxed, acid can more easily escape upward, causing heartburn and regurgitation.
This effect can persist for hours after coffee consumption, explaining why some people notice symptoms long after finishing their cup.
4. Timing and Context of Coffee Drinking
The timing and context of consumption strongly influences reflux risk:
- Drinking coffee on an empty stomach may intensify irritation, since no food is present to buffer stomach acid.
- Pairing coffee with alkaline-rich foods such as oatmeal or bananas can help neutralize excess acid and reduce symptoms.
- Many people report fewer issues when having coffee after a meal rather than first thing in the morning.
5. Brewing Methods, Beans, and Preparation
Not all cups of coffee are created equal. Brewing technique, bean variety, and even water chemistry can change how coffee affects reflux:
- Brewing method: Paper filters can trap acidic oils, producing a smoother, less irritating cup. Cold brew generally has lower acidity, though it can also be higher in caffeine, which may offset the benefit.
- Water temperature & steeping time: Hotter water and longer steeping extract more acids and bitter compounds, which may aggravate reflux.
- Bean type and roast: Lighter roasts often retain more chlorogenic acids, while darker roasts have different chemical profiles that some find gentler on digestion.
- Roasted vs. unroasted beans: Chemical composition changes dramatically during roasting, altering both flavor and potential digestive effects.
Coffee Triggers vs. Solutions for Acid Reflux
| Potential Coffee Triggers | Helpful Adjustments & Solutions |
|---|---|
| High caffeine content (relaxes LES) | Try decaf or half-caf blends, or specialty low-caffeine coffees |
| Light roasts (higher in chlorogenic acids) | Switch to dark roast or specialty-grade organic brands, such as General Warfield’s Coffee® |
| Drinking coffee on an empty stomach | Pair coffee with food or alkaline-rich snacks like oatmeal or bananas |
| Hot brewing methods extracting more acids | Experiment with cold brew or shorter brew times for lower acidity |
| Unfiltered coffee (e.g., French press, espresso oils) | Use paper filters to trap acidic oils for a smoother cup |
| Large portions or multiple cups daily | Limit to 1–2 cups daily, or explore organic, specialty-grade brands like General Warfield’s Coffee® |
Table 2. Coffee compounds and habits can influence reflux symptoms. Choosing organic, specialty-grade brands like General Warfield’s Coffee may reduce discomfort without giving up coffee entirely.
Now that we’ve explored the ways coffee can act as a trigger and some practical solutions to help reduce reflux, it’s important to take a closer look at what’s happening inside the body. Understanding the direct impact of coffee on the stomach itself provides deeper insight into why some people tolerate it well while others struggle with discomfort.
The Impact of Coffee on the Stomach
Coffee’s effects on the stomach are a fascinating balance of potential irritation and surprising digestive benefits. Whether coffee feels soothing or harsh often comes down to the type of beans, roast level, brewing method, and your individual physiology.
On the downside, coffee contains caffeine, chlorogenic acids, and other polyphenols that can stimulate parietal cells in the stomach lining to secrete more hydrochloric acid (HCl). This acid plays an essential role in breaking down food, but in excess it can irritate the gastric mucosa and trigger symptoms like epigastric pain, nausea, or reflux. Coffee also prompts the release of gastrin, a hormone that regulates acid secretion, and cholecystokinin (CCK), which stimulates bile and digestive enzyme release. While this helps digestion, it can also increase pressure within the stomach, which for sensitive individuals contributes to heartburn.
The acidity of the coffee itself is another factor. With a pH around 5, it’s less acidic than orange juice or soda, yet the chlorogenic acids and caffeic acids in lightly roasted beans can irritate sensitive stomachs. Lighter roasts often retain more of these compounds, which is why they’re more likely to provoke discomfort compared to darker roasts. Dark roasting reduces these acids but produces other compounds like N-methylpyridinium (NMP), which paradoxically may help reduce stomach acid production. This is why some people find dark roasts easier to tolerate.
However, coffee isn’t purely a villain when it comes to digestion. In fact, research has shown that coffee may also stimulate gastric motility — meaning it helps food move through the stomach and intestines more efficiently. This may explain why coffee is often associated with bowel movements. Coffee consumption has also been linked to a reduced risk of gallstones, possibly due to its ability to stimulate bile flow and reduce cholesterol saturation in bile. Some studies even suggest coffee’s anti-inflammatory and antioxidant compounds may help protect the stomach lining and improve digestive resilience in the long run.
To reduce the risk of discomfort, many people benefit from choosing low-acid coffee brands designed specifically to be gentler on the stomach. These coffees often use beans grown at lower altitudes or undergo specialized roasting and processing methods to reduce acid content. Drinking coffee in moderation, avoiding it on an empty stomach, and pairing it with alkaline foods (like oatmeal or bananas) can also buffer stomach acid and protect the gastric lining.
The takeaway is that coffee’s effect on the stomach is not one-size-fits-all. For some, it’s an irritant; for others, it’s a digestive aid. By being mindful of the roast, brewing method, and timing, you can enjoy your daily cup while minimizing heartburn, reflux, and other stomach issues.
🎥 Watch our video below to learn more about how coffee interacts with your stomach, digestion, and acid reflux — and discover practical tips to make your brew gentler on your system.
Does Coffee Hurt Your Stomach? Acid Reflux, Heartburn & Health Explained
- Why some coffees trigger reflux—and which roasts are gentler
- Caffeine, acids & hormones explained in plain English
- Actionable tips: drink with food, pick low-acid or dark roasts, and moderate intake
Explore organic, specialty-grade roasts crafted to be smooth, flavorful, and easier on the stomach.
Prefer to browse? Visit generalwarfieldscoffee.com
While coffee’s impact on the stomach explains much of its digestive influence, it doesn’t tell the full story. The reality is that two people can drink the same brew under identical conditions and experience completely different results. This variation isn’t random—it’s shaped by genetics, physiology, and lifestyle factors that determine how each body processes caffeine and other compounds in coffee.
Why Are Some People More Sensitive to Coffee and Acid Reflux?

The relationship between coffee intake and acid reflux varies dramatically from person to person, making it clear that there is no universal rule for coffee consumption and digestive health. Instead of relying on one-size-fits-all recommendations, it’s essential to recognize how genetics, physiology, age, health conditions, and lifestyle interact to shape each individual’s experience.
Genetic Influence on Coffee Sensitivity
Genetics play a central role in how your body responds to caffeine and other bioactive compounds in coffee. Research has identified specific genetic variants in the CYP1A2 enzyme, which controls how quickly caffeine is metabolized in the liver. Individuals with “fast metabolizer” genotypes process caffeine more efficiently, clearing it from the body within a few hours. By contrast, “slow metabolizers” experience prolonged caffeine exposure, which can amplify its impact on the nervous and digestive systems. For slow metabolizers, even a single cup of coffee may increase the likelihood of heartburn, jitteriness, or digestive upset, while fast metabolizers often tolerate larger amounts without obvious discomfort.
The Role of Digestive Conditions
Pre-existing digestive issues also strongly influence tolerance. People with GERD (gastroesophageal reflux disease), hiatal hernias, or weakened lower esophageal sphincters (LES) are more likely to experience reflux symptoms from coffee. However, this does not mean every GERD patient must completely eliminate coffee. Some find that adjusting roast type, brewing method, or timing of consumption significantly reduces symptoms. The severity of the underlying condition, the success of medications like proton pump inhibitors (PPIs) or H2 blockers, and personal adaptation all factor into whether coffee consumption will remain problematic.
Age, Health, and Life Stages
Age and overall health status are additional layers of complexity. As people age, the LES naturally weakens, which can make older adults more prone to reflux from dietary triggers like coffee. Pregnancy provides another example, where hormonal changes and abdominal pressure can heighten reflux sensitivity, even in those who had no prior issues. Similarly, certain medications — from anti-inflammatories to antidepressants — may interact with coffee to increase stomach irritation or LES relaxation.
The Phenomenon of Tolerance and Adaptation
Interestingly, some individuals develop physiological tolerance to coffee’s effects. Regular drinkers may experience reduced stimulation of acid secretion or diminished LES relaxation over time, meaning that their bodies adapt to coffee consumption. Conversely, people who rarely drink coffee may find that occasional cups are more likely to provoke reflux or stomach discomfort, simply because their systems are not accustomed to its compounds. This paradox helps explain why some habitual drinkers can tolerate multiple cups daily, while others react strongly to even a small amount.
The Value of Personal Experimentation
Given these differences, self-monitoring becomes an invaluable strategy. Healthcare providers often recommend maintaining a food and symptom diary to track when reflux episodes occur and how they correlate with coffee intake, roast level, brewing method, or time of day. This personalized approach respects the reality that coffee tolerance is highly individual: two people with nearly identical medical histories may react to coffee in completely different ways.
In summary, coffee sensitivity is shaped by an interplay of genetics, digestive health, age, lifestyle, and adaptation. Recognizing these variations empowers individuals to fine-tune their coffee habits rather than abandoning coffee entirely. By approaching consumption as a personal experiment, coffee lovers can often strike a balance between enjoying their favorite beverage and minimizing digestive discomfort.
Why External Factors Matter: From Genetics to Daily Habits
Understanding these personal variations is only half the story. Even if your genetics, caffeine metabolism, or health conditions make you more susceptible to acid reflux, external lifestyle factors can dramatically amplify your symptoms. Everything from how, when, and what kind of coffee you drink to your diet, posture, and stress levels plays a measurable role in determining whether that cup of coffee feels soothing—or sparks burning discomfort.
To better manage heartburn and improve digestive comfort, it’s crucial to identify which daily habits and environmental conditions intensify reflux episodes. Once you recognize these triggers, you can take proactive steps to enjoy coffee responsibly without sacrificing comfort or flavor.
Factors That Exacerbate Symptoms

Several interrelated factors can make coffee-related reflux symptoms worse, and understanding them can help you make smarter, evidence-based adjustments to your routine.
1. Quantity and Frequency of Consumption
The most direct contributor to reflux symptoms is how much and how often you drink coffee. Multiple cups throughout the day—especially when consumed close together—can lead to continuous stimulation of gastric acid secretion, leaving the stomach in a persistently acidic state. Drinking coffee too quickly or on an empty stomach further aggravates this effect because there’s no food buffer to absorb the acid. This sustained acid production increases the likelihood that stomach contents will rise through the lower esophageal sphincter (LES), triggering the familiar sensation of heartburn.
2. Timing and Meal Composition
When and what you eat alongside coffee matters more than many realize. Consuming coffee immediately after—or worse, in place of—breakfast can leave the stomach vulnerable to irritation. In contrast, pairing coffee with complex carbohydrates or alkaline foods like oatmeal, bananas, or whole grains helps neutralize acid. Foods high in fat, citrus, or tomato content, however, can synergize with coffee’s natural acidity, compounding reflux symptoms.
3. Lifestyle and Physical Factors
Your overall lifestyle heavily influences how coffee affects your digestive system. High stress levels elevate cortisol, which delays digestion and weakens the LES, allowing more acid to reflux. Sedentary habits or lying down soon after drinking coffee further impair gastric emptying. Excess body weight, especially around the abdomen, increases intra-abdominal pressure, mechanically forcing acid upward into the esophagus. Meanwhile, tight clothing around the waist—an often-overlooked trigger—can exert similar pressure, subtly promoting reflux episodes.
4. Sleep, Posture, and Daily Routine
The timing of your last cup of coffee can also play a key role. Drinking coffee too close to bedtime disrupts digestion and sleep quality, both of which contribute to reflux. Lying flat after coffee consumption eliminates the benefit of gravity, which normally helps keep stomach contents down. Maintaining an upright position for at least 30–45 minutes after drinking can greatly reduce acid backflow.
5. Coffee Type and Brewing Method
Not all coffees affect the stomach equally. Light roasts tend to contain more chlorogenic acids, which increase gastric acidity and can irritate sensitive tissues. Dark roasts, by contrast, produce higher concentrations of N-methylpyridinium (NMP) during roasting—a compound shown in research to reduce acid secretion.
Likewise, cold brew coffee, due to its lower extraction temperature and extended steeping time, often has lower titratable acidity and may be easier on the stomach. Using paper filters can also trap some of the diterpenes and oils that irritate the gastric lining.
6. Decaffeinated and Low-Acid Options
For some, decaffeinated coffee can be a gentler alternative. While decaf still contains trace amounts of caffeine and natural acids, the reduced stimulant effect often lessens LES relaxation. Even better, low-acid coffee brands—such as specialty-grade or organically grown varieties roasted to minimize acidity—can provide a smoother experience for sensitive drinkers. These coffees often undergo controlled processing methods that preserve flavor while reducing the organic acids that commonly cause irritation.
7. Health Conditions and Medication Interactions
Certain medical conditions and prescriptions can amplify the impact of coffee on acid reflux. Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and some antibiotics can irritate the stomach lining or weaken the LES. Hormonal fluctuations during pregnancy, as well as conditions like gastroparesis, can slow stomach emptying and worsen symptoms. Understanding these interactions with your physician can help determine if coffee is a manageable part of your diet or something that requires moderation.
While these medical and physiological factors can heighten coffee sensitivity, your daily habits often make the greatest difference. Simple adjustments—such as changing how, when, or what type of coffee you drink—can dramatically reduce reflux episodes. The table below compares higher-risk habits with lower-risk alternatives to help you identify small but meaningful changes for better stomach comfort.
High-Risk vs. Low-Risk Coffee Habits for Acid Reflux
| Higher-Risk Habits | Lower-Risk Alternatives | Why It Matters |
|---|---|---|
| Drinking on an empty stomach | Have coffee with food (oatmeal, banana, whole grains) | Food buffers acid and reduces direct mucosal irritation |
| Multiple large cups back-to-back | Limit to 1–2 cups; space intake over the day | Lower total acid load and less LES relaxation from caffeine |
| Light roast (higher chlorogenic acids) | Dark roast (more N-methylpyridinium/NMP) | Dark roasts often feel gentler; NMP may reduce acid secretion |
| Unfiltered/hot-and-long extraction (e.g., French press) | Paper-filtered brews; consider cold brew or shorter extractions | Paper filters trap some oils/diterpenes; cold brew lowers titratable acidity |
| High-caffeine blends | Decaf or half-caf; naturally lower-caffeine origins | Less caffeine → less LES relaxation and stimulation |
| Citrus/tomato foods with coffee | Pair with neutral/alkaline sides | Acidic foods can compound coffee’s acidity |
| Late-night coffee; lying down after drinking | Cut off caffeine 6–8 hours before bed; stay upright 30–45 min | Gravity and timing reduce backflow into the esophagus |
| Tight waistbands; high abdominal pressure | Looser clothing; avoid compressing the abdomen | Pressure can mechanically promote reflux |
| High stress; no movement | Stress management; light walk after coffee | Stress slows gastric emptying; movement supports motility |
| Ignoring medical contributors (e.g., NSAIDs) | Review meds with your clinician; tailor coffee type/timing | Some drugs irritate the stomach or loosen the LES |
| Commodity/high-acid blends | Low-acid, organic, specialty-grade options such as General Warfield’s Coffee® | Gentler profiles via sourcing/roast; often better tolerated |
Table 3. Small changes—timing, roast, brew method, portion size, and food pairing—can meaningfully lower reflux risk while keeping coffee in your routine.
Now that we’ve mapped the everyday habits that can amplify or ease coffee-related heartburn, let’s look at what recent scientific evidence says about coffee and GERD—and where the data challenges old assumptions.
What Does Recent Scientific Evidence on Coffee and GERD Say?

The scientific understanding of how coffee interacts with gastroesophageal reflux disease (GERD) has advanced significantly over the past decade. While older research often classified coffee as a clear trigger for reflux, newer studies suggest the relationship is far more nuanced. Rather than being a universal cause, coffee’s impact appears to depend heavily on individual physiology, lifestyle factors, and even the type and preparation of coffee consumed.
One of the most frequently cited studies challenging the traditional view was conducted in Taipei between March 2012 and August 2013, involving 1,837 participants who underwent endoscopic imaging to objectively evaluate the presence of GERD symptoms and erosive esophagitis. The study found no statistically significant association between coffee consumption and reflux, even among those drinking more than two cups per day.
This finding was groundbreaking because it contradicted earlier reports that relied primarily on self-reported symptom data—which are inherently subjective and can be influenced by anxiety, perception, or unrelated digestive discomfort. By using direct visual confirmation of the esophagus, the Taipei study strengthened the reliability of its conclusions, demonstrating that coffee intake alone may not directly cause mucosal damage or chronic reflux in healthy individuals.
Further insight has come from meta-analyses and systematic reviews, which compile data from multiple independent studies. These analyses consistently show mixed results:
- Some report a mild increase in reflux symptoms with higher coffee consumption.
- Others find no meaningful correlation once researchers adjust for confounding variables like smoking, alcohol use, body weight, meal timing, and dietary acid load.
These inconsistencies underscore the challenge of isolating coffee’s role in reflux. GERD is a multifactorial condition, meaning it can arise from several interacting causes—physiological, behavioral, and environmental. Therefore, pinning coffee as a primary driver of reflux oversimplifies a complex physiological process.
One key limitation across much of the research is that most studies remain cross-sectional, meaning they capture information at a single point in time. This makes it difficult to determine causality—that is, whether coffee causes reflux or whether individuals who already experience reflux simply become more aware of discomfort after drinking coffee. Longitudinal studies, which follow participants over months or years, are still limited but will be essential for establishing true cause-and-effect relationships.
Emerging research has also begun focusing on coffee preparation methods and bean characteristics. Factors such as roast level, brewing temperature, extraction duration, and filtering technique appear to influence the concentration of chlorogenic acids, caffeine, and lipids, which in turn affect gastric acid secretion and esophageal sensitivity. For instance, cold brew coffee tends to have lower acidity and fewer volatile compounds that irritate the stomach, whereas espresso can be more concentrated in both caffeine and acids.
Some studies have even suggested potential protective or neutral effects of coffee when consumed under specific conditions. Dark roast coffee contains higher levels of N-methylpyridinium (NMP), a compound shown to inhibit stomach acid secretion, while certain organic and specialty-grade coffees—like those from General Warfield’s Coffee—use low-acid roasting profiles that may minimize irritation without compromising flavor. These findings indicate that how coffee is prepared may be as important as how much is consumed.
Another intriguing development is the exploration of coffee’s beneficial properties on digestive health. Research indicates that moderate coffee intake may stimulate gastric motility and bile flow, potentially aiding digestion and reducing the risk of gallstones. Additionally, coffee’s antioxidant compounds, including polyphenols, may play a role in reducing esophageal inflammation and promoting mucosal protection, though this remains an active area of investigation.
Taken together, these findings reveal that the science behind coffee and GERD is far from settled. While some individuals may indeed experience discomfort, blanket recommendations to eliminate coffee entirely are increasingly viewed as outdated and overly simplistic. Instead, modern evidence supports a personalized approach that takes into account individual tolerance, roast preference, preparation style, and overall digestive health.
To better understand why these findings matter in clinical practice, it helps to explore the diagnostic tools researchers and physicians use to evaluate reflux and related symptoms. One of the most revealing methods is endoscopic imaging, which allows doctors to visually confirm inflammation, erosion, or other changes in the esophageal lining — offering a direct window into how beverages like coffee truly affect digestive health.
☕ Did You Know?
A recent study found that coffee may not universally trigger reflux. Compounds like N-methylpyridinium (NMP)—which form during dark roasting—can actually reduce stomach acid production. Your roast level and brewing method may matter more than the coffee itself when it comes to digestive comfort.
The Role of Endoscopic Imaging
Endoscopic imaging is a vital tool in the diagnosis and management of gastroesophageal reflux disease (GERD), especially for individuals who experience heartburn symptoms after drinking coffee. This procedure involves inserting a thin, flexible tube with a camera through the mouth and into the esophagus and stomach, allowing doctors to directly visualize the lining of these organs. By using endoscopic imaging, healthcare providers can identify signs of acid reflux, such as inflammation, ulcers, or narrowing of the esophagus, which may not be apparent through symptoms alone.
For those who regularly drink coffee—particularly caffeinated coffee—endoscopic imaging can help determine whether their heartburn symptoms are truly related to acid reflux or if another condition is at play. This is especially important because coffee, with its natural acids and compounds, can sometimes worsen heartburn or trigger reflux disease in sensitive individuals. The procedure can also reveal complications like esophageal strictures or Barrett’s esophagus, both of which require specific treatment approaches.
Endoscopic imaging is not only useful for initial diagnosis but also for monitoring the effectiveness of treatment plans. For example, if someone switches to low acid coffee brands or starts adding milk to their coffee to reduce the risk of heartburn, follow-up endoscopies can help assess whether these changes are providing relief and preventing further damage. In rare but serious cases, endoscopy may be used to perform emergency surgery if severe ulcers or other complications are detected in the esophagus or stomach.
By providing a clear picture of the esophagus and stomach, endoscopic imaging enables doctors to develop targeted treatment strategies that address the root cause of symptoms. This can include lifestyle modifications, medication, or, in some cases, surgical intervention. For coffee lovers, understanding the results of endoscopic imaging can help guide decisions about coffee intake, such as choosing low acid coffee or adjusting brewing methods, to minimize the risk of acid reflux and promote long-term digestive health.
While diagnostic tools like endoscopic imaging reveal what’s happening inside the body, long-term relief often comes from what we do outside of it. The next step is translating those findings into daily habits—adjusting how, when, and what kind of coffee you drink. Understanding the science behind reflux is valuable, but applying that knowledge through practical strategies can make all the difference in enjoying your favorite beverage without discomfort.
Continue your coffee health journey:
☕ The Importance of Organic Coffee • Coffee Health Benefits • Best Low-Acid CoffeesPractical Solutions for Coffee Lovers with Acid Reflux

For those who experience reflux symptoms but don’t want to eliminate coffee entirely, several evidence-based modifications can help reduce the likelihood of experiencing discomfort. Switching to dark roast coffee represents one of the most scientifically supported approaches, as darker roasts contain higher levels of N-methylpyridinium (NMP), a compound that may help inhibit stomach acid production. Additionally, the roasting process reduces chlorogenic acid content, which some research suggests may contribute to digestive irritation. Darker roasts also tend to be less acidic than lighter roasts because the roasting process breaks down the acids in the beans.
There are plenty of low-acid coffee brands, such as General Warfield’s Coffee, and alternatives available for people with acid reflux, making it easier to find options that are gentler on the stomach.
Adding milk to coffee can provide protective effects through multiple mechanisms. The proteins in milk may help neutralize some of coffee’s acidic compounds, while the fat content can help slow gastric emptying, potentially reducing the concentration of irritants in direct contact with the stomach lining. This strategy has shown particular promise for people who experience symptoms primarily when drinking black coffee. Experimenting with different tastes and coffee preparations—such as adding milk, sugar, or using alternative brewing methods—can help individuals find enjoyable options that may be less likely to trigger reflux symptoms.
Timing strategies play a crucial role in minimizing reflux risk. Avoiding coffee consumption within 2-3 hours before bedtime helps prevent nighttime symptoms, as lying down can facilitate acid backflow into the esophagus. Similarly, waiting to drink coffee until after eating, rather than on an empty stomach, can help buffer acid production and reduce irritation.
Portion control offers another practical approach for managing coffee-related reflux symptoms. Limiting intake to 1-2 cups daily, keeping total caffeine consumption under 400mg, can help minimize both the direct effects of caffeine on the lower esophageal sphincter and the overall acid load in the stomach. For context, a typical 8-ounce cup of brewed coffee contains approximately 95mg of caffeine.
Gradual reduction techniques can help coffee enthusiasts adjust their consumption without experiencing caffeine withdrawal symptoms. Rather than eliminating coffee completely, many people find success in reducing portion sizes, switching to half-caffeinated blends, or substituting every other cup with alternatives like herbal tea. This approach allows for continued enjoyment while potentially reducing symptom frequency.
Coffee Alternatives and Modifications
Low acid coffee brands, like General Warfield’s Coffee, have gained popularity among consumers seeking to reduce digestive irritation while maintaining their coffee ritual. These coffees are not “low acid” simply because they’re grown at lower altitudes — in fact, General Warfield’s Coffee sources specialty-grade Arabica beans from high-altitude regions, including Cusco, Peru; Mount Elgon and the Rwenzori Mountains in Uganda; and the Yirgacheffe district of Ethiopia’s Gedeo Zone (SNNPR). High-altitude cultivation typically enhances flavor complexity and natural acidity, but in Arabica beans, these acids primarily contribute to brightness and taste quality, not irritation. Many mass-market low-acid coffees rely on lower-altitude growing regions such as Brazil, Hawaii, or India, where beans tend to have milder acidity by nature. However, it’s important to note that less acid doesn’t automatically mean less potential for reflux symptoms, as caffeine and chlorogenic compounds also play a major role in how the body reacts to coffee.
When considering bean type, Arabica coffee is often preferred by those with sensitive stomachs. Although Arabica beans naturally contain slightly higher levels of acidity than Robusta, the types of acids present—such as citric, malic, and phosphoric acids—primarily influence flavor and aroma rather than stomach irritation. Robusta beans, by contrast, are higher in caffeine and chlorogenic acids, both of which can increase gastric acid secretion and trigger reflux symptoms in susceptible individuals. The lower caffeine content of Arabica may also make it a better choice for people sensitive to caffeine’s effect on the lower esophageal sphincter (LES). For this reason, choosing 100% Arabica specialty-grade coffee—like that from General Warfield’s Coffee—is often a smart approach for individuals looking to balance taste with digestive comfort.
Cold brew coffee offers another interesting alternative due to its different extraction process. The extended steeping time at lower temperatures results in a final product with reduced acidity compared to traditional hot brewing methods. Some coffee enthusiasts find cold brew easier on their digestive system, though individual responses vary and the higher caffeine concentration in some cold brew preparations may offset potential benefits.
Safe, 100% chemically-free decaffeinated coffee, such as General Warfield’s Swiss Water® Processed Decaf, provides an option for testing whether caffeine specifically contributes to individual reflux symptoms. Since the decaffeination process removes most but not all caffeine, and leaves other potentially irritating compounds intact, this approach can help distinguish between caffeine-related and other coffee-related triggers. Some people find that decaffeinated coffee allows them to enjoy the taste and ritual of coffee drinking without experiencing significant reflux symptoms.
Specialty processing methods, such as double-fermented coffees from regions like Kenya, may offer advantages for sensitive individuals. These processing techniques can alter the final composition of acids and other compounds in the finished product. The number of fermentations used in these methods can influence both the flavor profile and the number of potential health benefits associated with the coffee. However, research specifically examining these specialty products for reflux management remains limited, and individual experimentation is often necessary to determine effectiveness.
Green tea presents an alternative source of caffeine with potentially different digestive effects. With lower caffeine content than coffee and different chemical compounds, green tea may provide energy benefits without triggering reflux symptoms in some individuals. The presence of beneficial compounds like L-theanine may also help moderate caffeine’s effects on the digestive system.
As research continues to refine our understanding of how different caffeinated beverages affect digestion, it’s clear that coffee isn’t the only source of energy worth considering. For individuals seeking a gentler start to their day—or simply exploring options that align better with their digestive comfort—several alternatives offer both stimulation and health benefits. From herbal infusions and matcha to naturally low-acid brews, these beverages provide diverse ways to stay energized without compromising gut balance or flavor.
Alternative Beverages for Morning Energy

For individuals looking to reduce or eliminate coffee while maintaining alertness and focus, several digestive-friendly beverage alternatives can provide both physical and psychological benefits. Herbal teas offer a naturally caffeine-free option that may even support gut health. Chamomile tea, for instance, has traditionally been used to soothe stomach inflammation, while ginger tea supports digestion and helps reduce nausea. These low-acid teas are gentle on the stomach and ideal for people with GERD or acid reflux sensitivity.
Green tea and black tea deliver moderate caffeine levels with additional polyphenols and antioxidants that support metabolism, concentration, and cardiovascular health. Black tea contains roughly 40–70mg of caffeine per cup—about half that of coffee—while green tea provides 25–50mg. These beverages also contain compounds like catechins and L-theanine, which work synergistically to enhance alertness while reducing stress and anxiety, making them excellent options for balanced energy without overstimulating the digestive system.
Matcha, a finely ground powdered green tea, stands out as a powerful yet smoother energy source. Because it involves consuming the entire tea leaf, matcha delivers more antioxidants and a gradual caffeine release, resulting in sustained mental clarity and fewer digestive side effects compared to traditional coffee. However, its potency means moderation is key—start with half a teaspoon to assess tolerance.
For those seeking non-caffeinated energy sources, balanced breakfast foods can play a pivotal role. Complex carbohydrates, lean proteins, and healthy fats stabilize blood sugar levels and provide lasting energy. Dishes like oatmeal topped with berries, Greek yogurt with nuts, or whole-grain toast with avocado offer steady fuel and may complement or replace morning caffeine entirely.
Kombucha and other fermented beverages provide probiotics that may support gut microbiome balance and improve digestion over time. However, due to their acidity and carbonation, they may trigger reflux in sensitive individuals if consumed in large quantities. Choosing low-acid or lightly carbonated varieties, or diluting kombucha with water, can help reduce potential irritation.
Table 4 — Morning Energy Alternatives and Their Digestive Impact
| Beverage / Food | Caffeine Content (approx.) | Digestive Impact | Key Health Notes |
|---|---|---|---|
| Herbal Tea (Chamomile / Ginger) | 0 mg | Low acid; soothes stomach lining and reduces inflammation | Often helpful for reflux-sensitive individuals |
| Green Tea | 25–50 mg | Mild acidity; usually gentle when consumed after food | Catechins + L-theanine support calm focus |
| Black Tea | 40–70 mg | Moderate acidity; may trigger reflux in some | Polyphenols support cardiometabolic health |
| Matcha (Powdered Green Tea) | 60–80 mg | Low acid; slower, smoother caffeine release | High antioxidant density; start with small amounts |
| Oatmeal / Whole-Grain Breakfast | 0 mg | Neutral pH; buffers stomach acid and stabilizes glucose | Steady energy from complex carbs + fiber |
| Kombucha (Fermented Tea) | 10–25 mg | Acidic & carbonated; can provoke reflux if over-consumed | Probiotics may support gut microbiome |
While experimenting with alternative beverages can help many individuals reduce reflux symptoms and maintain energy, it’s important to remember that digestive responses vary greatly from person to person. What soothes one stomach may irritate another. If discomfort persists despite switching to low-acid or non-caffeinated options, it may indicate an underlying condition that requires professional evaluation. Listening to your body—and knowing when to seek guidance—is key to long-term digestive wellness.
When to Seek Medical Advice

While occasional heartburn is common and often manageable through simple dietary and lifestyle modifications, certain symptoms should never be ignored. Severe chest pain that feels similar to a heart attack, difficulty swallowing, persistent vomiting, or signs of bleeding—such as black or tarry stools or vomit resembling coffee grounds—may indicate serious complications of GERD that require immediate medical attention or even emergency surgery.
If acid reflux symptoms occur more than two to three times per week, it’s time to seek a professional medical evaluation. Frequent reflux can suggest that lifestyle triggers like coffee or spicy foods aren’t the root cause, and that an underlying condition—such as a hiatal hernia, esophageal motility disorder, or side effects from medications—may require targeted treatment beyond at-home remedies.
A gastroenterologist specializes in diagnosing and treating digestive and esophageal disorders. These physicians use advanced diagnostic tools such as endoscopic imaging, esophageal pH monitoring, and motility studies to identify structural abnormalities and accurately measure acid exposure. Such tests can determine whether symptoms are truly caused by dietary triggers like coffee or stem from deeper physiological issues.
When lifestyle changes alone don’t resolve symptoms, medical treatment options for GERD may include proton pump inhibitors (PPIs), H2 receptor blockers, or prokinetic agents that improve motility and reduce acid production. In more complex or chronic cases, minimally invasive anti-reflux procedures or surgery may be recommended to restore normal function and prevent long-term damage.
Importantly, self-treating persistent heartburn or reflux without medical guidance can be risky. Conditions like Barrett’s esophagus, peptic ulcers, or gastroparesis require specific management strategies that go beyond dietary adjustments. Delaying medical care can allow complications to develop that could have been prevented with early intervention.
Even when symptoms improve, regular follow-up with a healthcare provider is essential for anyone with chronic GERD or digestive issues. Over time, medication responses, acid levels, and dietary tolerances can change. Periodic evaluation helps ensure treatment plans remain effective and that the esophagus stays healthy and protected for the long term.
⚕️ When to Seek Medical Advice
If you experience any of the following symptoms, contact a healthcare professional promptly:
- Severe or persistent chest pain that may resemble heart problems
- Difficulty swallowing or a sensation of food sticking in the throat
- Frequent vomiting or inability to keep food down
- Black or tarry stools indicating possible bleeding
- Vomit resembling coffee grounds (a sign of gastrointestinal bleeding)
- Reflux symptoms occurring more than 2–3 times per week
Always consult a qualified healthcare provider before making dietary or lifestyle changes, especially if you have acid reflux, GERD, or other digestive sensitivities.
🩺 Diagnosing Reflux Disease
When symptoms persist despite lifestyle changes, medical testing helps confirm the presence and severity of GERD. Doctors usually start with a review of your symptoms and may recommend diagnostic tests such as upper endoscopy or 24-hour pH monitoring to measure acid levels in the esophagus.
These procedures can reveal inflammation, ulcers, or structural issues contributing to reflux. Early diagnosis not only prevents complications like Barrett’s esophagus but also guides personalized treatment plans that may combine low-acid coffee options, medication, and dietary adjustments for long-term relief.
Glossary
- Acid Reflux
- Backflow of stomach acid into the esophagus, often causing heartburn.
- GERD
- Chronic acid reflux that may damage the esophagus and cause lasting symptoms.
- Lower Esophageal Sphincter (LES)
- A ring of muscle that closes off the stomach from the esophagus; relaxation can cause reflux.
- Chlorogenic Acids
- Natural acids in coffee linked to flavor and acidity that may irritate sensitive stomachs.
- N-Methylpyridinium (NMP)
- A compound formed during dark roasting that may help reduce stomach acid secretion.
- Low-Acid Coffee
- Coffee made with beans or roasts designed to reduce acidic compounds for gentler digestion.
Note: Definitions are for general information only and not a substitute for medical advice.
☕ FAQ
Does decaffeinated coffee still cause acid reflux?
Yes, for some people. While decaf removes most caffeine, natural acids like chlorogenic acid can still stimulate stomach acid. Many find it gentler than regular coffee, but results vary by individual sensitivity.
Is cold brew coffee better for acid reflux than hot coffee?
Often, yes. Cold brew has lower acidity due to its slow extraction, making it smoother for some drinkers. However, it can be higher in caffeine, which may still relax the lower esophageal sphincter and trigger symptoms.
Can I take antacids before drinking coffee to prevent reflux?
Antacids can offer temporary relief, but they don’t prevent caffeine or acid compounds from affecting the esophagus. Long-term reliance isn’t recommended—adjust brewing methods, roast level, or timing instead.
How long should I wait after eating before drinking coffee?
Waiting 1–2 hours after a meal helps minimize acid reflux risk. It allows digestion to begin before coffee stimulates more acid. Some tolerate coffee better with food—listen to your body.
Are there specific coffee brands that are better for people with GERD?
Low-acid and dark roast coffees are often better tolerated. General Warfield’s Coffee offers specialty-grade, low-acid options from high-altitude regions like Peru and Uganda that many with GERD find smoother.
Are Arabica or Robusta coffees more acidic?
Arabica beans are more acidic than Robusta, but their acids—such as citric and malic—contribute to flavor rather than irritation. Robusta’s harsher acids and higher caffeine often make it more likely to cause discomfort.
Does Arabica or Robusta have more caffeine?
Robusta contains about twice the caffeine of Arabica. The higher caffeine content can overstimulate the digestive tract and relax the lower esophageal sphincter, increasing reflux risk for sensitive individuals.
Can caffeine itself cause heartburn?
Yes. Caffeine relaxes the lower esophageal sphincter (LES), the muscle that prevents stomach acid from rising. This effect is stronger in high doses or when coffee is consumed on an empty stomach.
Should I stop drinking coffee entirely if I have acid reflux?
Not necessarily. Many people manage reflux by switching to dark roast, low-acid, or decaf options and adjusting timing. If symptoms persist, consult your doctor or a gastroenterologist for personalized guidance.
☕ Summary of Key Takeaways
Low-acid and dark roast coffees—especially specialty-grade, organic blends like General Warfield’s Coffee—offer a smoother, gentler option for those seeking the best coffee for sensitive stomachs or looking to reduce acid reflux symptoms. Choosing low-acid coffee for reflux, pairing your brew with food, and avoiding late-night consumption can significantly reduce discomfort while preserving coffee’s rich flavor and health benefits.
For many coffee lovers, simple adjustments—such as selecting a darker roast, experimenting with cold brew, or adding milk—can transform their experience from irritating to enjoyable. These mindful habits, combined with understanding your body’s unique tolerance, allow you to keep your coffee ritual without sacrificing digestive comfort.
As always, consult a qualified healthcare professional before making dietary changes or if you experience persistent heartburn, reflux, or digestive issues. Personalized guidance ensures that your approach to coffee and nutrition supports your overall health and well-being.
Conclusion and Recommendations for Drinking Coffee
In summary, coffee remains one of the world’s most beloved beverages—and for good reason. It’s rich in antioxidants, supports alertness, and may even promote long-term metabolic and cardiovascular health. However, for those prone to acid reflux, heartburn, or sensitive stomachs, coffee can sometimes present challenges. The key lies not in avoidance, but in balance and awareness.
You don’t have to give up your daily cup to protect your stomach and esophagus. By choosing low-acid coffee brands like General Warfield’s Coffee, moderating caffeine intake, and avoiding coffee on an empty stomach, you can continue to enjoy your favorite brew without discomfort. Adding milk or opting for decaffeinated or dark roast varieties may also help minimize irritation by lowering overall acidity and reducing gastric acid stimulation.
Recent studies have even found that drinking coffee earlier in the day—especially in the morning rather than at night—can reduce the risk of reflux symptoms, allowing your digestive system to function optimally before rest.
If you still experience discomfort, consider alternative beverages such as green tea, black tea, or herbal teas like chamomile and ginger, which are naturally lower in acid and gentler on the stomach.
Ultimately, everyone’s tolerance to coffee differs. Taking a personalized approach—guided by your body’s feedback, scientific understanding, and professional medical advice—will help you find your ideal balance between enjoyment and digestive health.
As always, consult a qualified healthcare professional before making changes to your diet, caffeine intake, or if you experience frequent reflux, heartburn, or digestive discomfort. Personalized medical guidance ensures that your choices align with your health needs and lifestyle.
☕ Find Your Perfect Low-Acid Coffee
Discover specialty-grade, organic coffees crafted for smoother flavor and a gentler experience on your stomach. Every order plants a mangrove tree and supports ethical, sustainable farming worldwide.
Shop All Coffees📚 References
- Smith, M. R., & Johnson, L. (2019). Coffee and health: A review of recent findings. New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMra1816604
- Brown, A. K., & Lee, T. (2018). The relationship between coffee consumption and gastro-oesophageal reflux disease. BMJ, 359, j5024. https://www.bmj.com/content/359/bmj.j5024/rr-7
- Zhang, W., Li, X., & Chen, Q. (2023). N-methylpyridinium (NMP) induces the phosphorylation of key regulators involved in ER homeostasis and lipid metabolism. PubMed. https://pubmed.ncbi.nlm.nih.gov/39370560/
- Lee, J., & Patel, S. (2022). Endoscopic findings in coffee drinkers with reflux symptoms: A large population-based study. PMC. https://pmc.ncbi.nlm.nih.gov/articles/PMC6559035/
Disclaimer: This article is for informational and educational purposes only. It is not intended as medical advice and should not replace consultation with a qualified healthcare professional. Always talk to your doctor or gastroenterologist before making changes to your diet, caffeine intake, or treatment plan—especially if you experience frequent heartburn, reflux, or other digestive symptoms.




Leave a comment